Does Your Child Really Need a Tonsillectomy? What Parents Should Know Before Saying Yes
Tonsillectomies the surgical removal of the tonsils have long been one of the most common operations performed on children. Yet in recent decades, doctors and parents alike have started asking a crucial question: Is surgery always the best answer?

Back in the 1960s, nearly a million children under 15 had their tonsils removed each year. But by 2006, that number had been cut in half. By 2010, it had been halved again. The reason for this sharp decline isn’t mysterious, it's caution. While tonsillectomies can bring real relief, they also come with risks that families should weigh carefully.
Why Fewer Tonsillectomies Are Being Done
Modern medicine has grown more conservative when it comes to removing tonsils. We now know that about one in five children experiences some kind of complication after a tonsillectomy.
Breathing difficulties are the most common, affecting roughly one in ten children.
Bleeding occurs in about one in twenty cases, and it can happen several days after surgery sometimes after the child has already gone home.
Deaths are thankfully extremely rare, but even minor complications can be frightening. That’s why most pediatricians now view tonsillectomy as a last resort, not an automatic fix.
The Two Principal Causes of Tonsillectomy
For two main reasons, doctors typically advise tonsil removal:
when breathing becomes difficult due to swollen tonsils (particularly during sleep).
When a child suffers from repeated, severe throat infections.
But as with many medical decisions, the details are rarely black and white.Let us examine both scenarios.
1.Tonsillectomy for Obstruction in Breathing
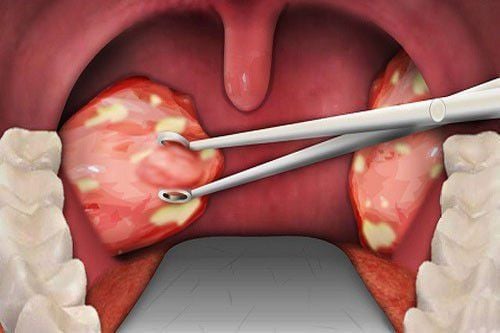
Adenoids and tonsils can occasionally enlarge to the point that they obstruct a child's airway, particularly when they are lying down. Obstructive sleep apnea (OSA), a disorder when a child stops breathing for brief periods of time while they sleep, may result from this.
Note that your child does not necessarily have apnea just because they snore. Parents should keep an ear out for breathing pauses that are frequently followed by choking or gasping noises. Poor sleep, exhaustion, irritation, and even behavioral problems during the day might result from these episodes.
When the Decision Is Clear
If a child’s tonsils are visibly huge and the symptoms are obvious (many parents now record sleep videos on their phones to show doctors), surgery often makes an immediate and dramatic difference.
When the Decision Is Not So Clear
Other times, the picture is murkier especially when the tonsils aren’t very large or the symptoms are mild. In such cases, doctors may recommend a sleep study, known as a polysomnogram (PSG). This overnight test monitors breathing patterns, oxygen levels, and sleep quality.
PSGs can be incredibly informative, but they’re not perfect. They only capture one night’s data, and sleep quality can vary. They also don’t always predict whether surgery will actually solve the problem particularly in overweight children, for whom apnea may persist even after tonsil removal.
Because PSGs are expensive and not always available, doctors’ opinions differ on when to order them and how to interpret the results.
Non-Surgical Options
Other choices are available if surgery seems hazardous or premature:
Devices for Continuous Positive Airway Pressure (CPAP)
The use of positional treatment to promote side sleeping
When necessary, weight control and medication
These can be quite successful for certain families without requiring surgery at all.
2. Recurrent Throat Infections: Tonsillectomy
Children who frequently get serious throat infections are the second main reason why doctors think about tonsil ectomy.
But “frequent” and “severe” have specific medical definitions.
A tonsillectomy might be considered if a child has:
7 or more infections in one year, or
5 infections each year for two consecutive years, or
3 infections per year for three years in a row.
And to count, these infections must involve fever, swollen lymph nodes, pus on the tonsils, or a positive strep test, not just a sore throat.
Even then, research shows something interesting: children who don’t get their tonsils removed often improve naturally over time. Their immune systems mature, and the infections taper off. Doctors sometimes call this the “tincture of time” , a reminder that patience can be powerful medicine too.
Balancing Risks, Relief, and Reality
So, should your child have a tonsillectomy? There’s no one-size-fits-all answer. For some children, especially those struggling with serious sleep obstruction, the surgery can be life-changing.Others might be better off waiting, keeping an eye on, and controlling their symptoms.
Before deciding, have an honest conversation with your child's doctor or an ENT specialist.
What's Your Reaction?